The demand for GLP-1 medications keeps climbing—and so do the costs. As the benefits landscape continues to shift, weight management has become one of the most challenging areas to get right. GLP-1s have redefined what’s possible for metabolic health—but they’ve also introduced new pressures for employers trying to balance impact and affordability. For employers it’s not a question of whether to act, but how to adjust their GLP-1 benefits strategy. How can they adjust to these rising costs and employee demand?
A changing field for weight management
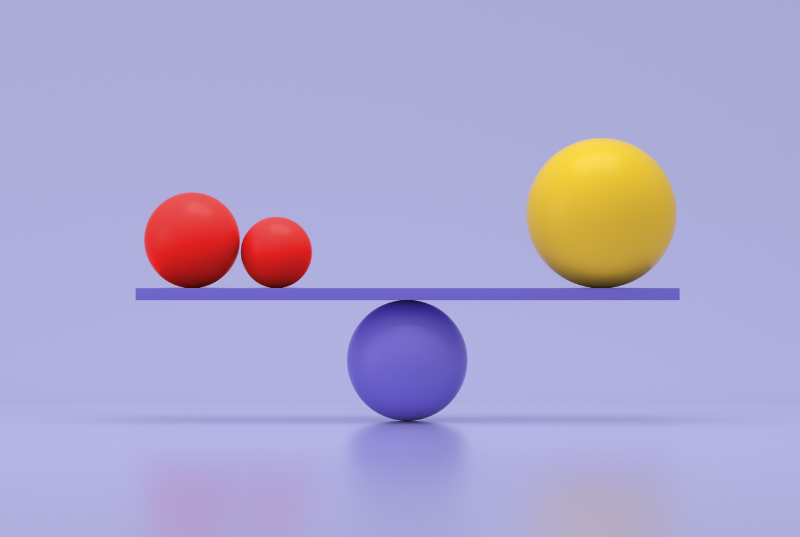
GLP-1 medications have reshaped obesity care and redefined the cost game for employers. The opportunity is clear, but so are the pressures: strong clinical outcomes on one side and escalating spend on the other.
Recent surveys show what employers are up against:
- Pharmacy spending now accounts for nearly a quarter of total healthcare costs.
- Two-thirds of employers cover or are considering coverage for GLP-1s, yet cost containment remains the top concern.
- Some are exploring new plan structures, including self-pay options, to improve access without increasing claims exposure.
Employees want credible, comprehensive support for their metabolic health. Employers need solutions that deliver it responsibly. The most effective strategies are the ones built to flex as treatments, costs, and workforce needs evolve.
Flexibility as a foundation
More organizations are turning to configurable programs that align care with cost.
Our own program is designed to cover the full-spectrum of care and work across coverage models—employer-sponsored and employee self-pay—so employers can offer evidence-based support without adding financial risk.
That configurability keeps benefits flexible as needs shift and gives employers more choice and cost control while improving care quality and access.
Self-pay: expanding access, containing cost
An employee self-pay GLP-1 coverage option gives employees clinically guided access to medication while keeping costs contained. Benefits include:
- No added employer cost: Participants pay out of pocket, keeping claims flat and plan budgets steady.
- Broader access: Extends care to people who don’t have GLP-1 coverage but still qualify and can benefit from treatment.
- Tiered support: Meets each participant where they are—whether through behavior-change support alone or in combination with medication—to create a personalized path to progress.
- Clinically guided care: Coordinates medical providers, nutrition experts, and behavior-change coaches to ensure safe, sustainable results.
- Benefit perception: Reinforces the organization’s commitment to practical, whole-person health—not just short-term solutions.
This model balances cost and control, supporting both employee outcomes and organizational goals.
A benefits strategy built to last
Sustaining effective obesity care requires flexibility and foresight. Employers that design benefits around configurable options—anchored in behavior change and clinical oversight—are better positioned to manage GLP-1 costs and maintain long-term impact.
In a field that’s constantly changing, the strongest strategies are the ones built to adjust and stay in the game.
See how Wondr Health can help your organization protect your team and stay in the game for the long run. Visit https://go.wondrhealth.com/winningapproach to learn more.