Weight-loss medications have taken center stage in obesity and chronic condition care—and they’re not slowing down anytime soon. As new indications emerge and oral versions move closer to market, it’s no surprise that employers are reevaluating their benefit strategies. But many of those strategies focus more on access than what happens next.
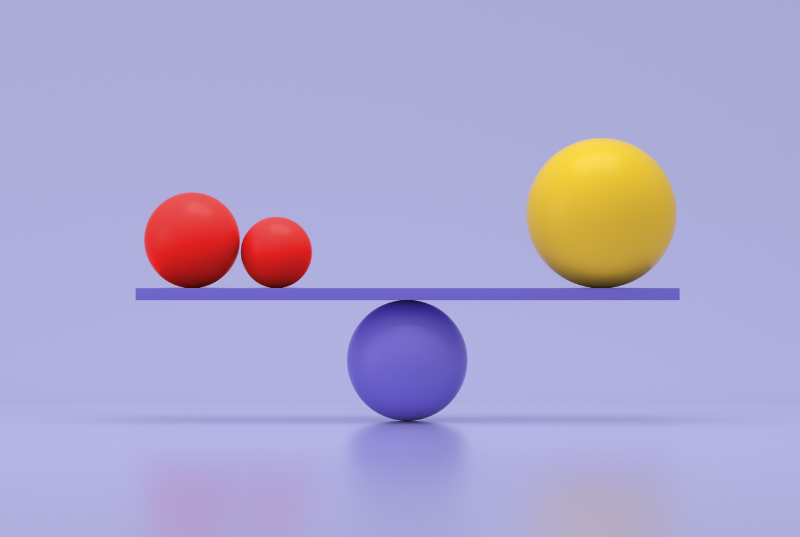
Medications can be powerful tools, not complete strategies.
More and more organizations are stepping up to offer access to GLP-1s. But access without structure rarely leads to lasting results. The real challenge (and opportunity) lies in what happens after the prescription is filled.
This is especially apparent when you look at the numbers. While clinical trial adherence is over 85%, the real-world numbers tell a different story. Nearly 30% of users quit within the first month and over 70% discontinued within two years. It’s not a matter of coverage; it’s having a solid foundation of support throughout the GLP-1 stages.
Future-proofing means supporting every stage of the journey
Behavior change isn’t a box to check at the start—it’s the thread that runs through the entire GLP-1 experience. At Wondr Health, we’ve seen how each phase brings new challenges, and how ongoing support can make the difference between short-term progress and long-term transformation.
Here’s what that looks like in practice:
1. Before (or alongside) medication: Laying the behavior-change foundation
Some people start with behavior change, others begin medication first, and many do both at the same time. Or some will opt out of medication entirely. Regardless of where someone begins, early behavioral and lifestyle support can make progress more effective and lasting.
2. Early phase: Support for common, early challenges
Whether it lasts a few weeks or several months, the early phase of taking a GLP-1 can feel unpredictable. Titration, side effects, and the pressure to see immediate results often lead to doubt – and for some, discontinuation. The first few months are also when users are at the highest risk for discontinuation. This is a critical time for tactics such as behavioral and lifestyle support, expert guidance, personalized nutrition counseling, and tailored medication management.
3. Middle phase: Handling identity shifts and external pressure
We don’t talk enough about the middle of the journey. As people lose weight, new challenges surface—such as unsolicited comments from others, pressure to maintain progress, or just plain uncertainty about what comes next. This is a critical point where the right support can help people manage expectations, handle social dynamics, and keep building habits that stick.
4. Long-term: Maintenance and resilience
Does hitting a goal weight mean support is no longer needed? Absolutely not. This phase is about finding what works for the long haul—whether that’s adjusting to a final dose, transitioning off medication, building life-long habits, or learning how to manage setbacks when life shifts. It’s not about perfection. It’s about figuring out your formula for health going forward.
The importance of supporting the full population—not just GLP-1 users
And of course, GLP-1s may be in the spotlight but they’re only a portion of the population. Whether due to eligibility, personal preference, cost, or side effects, there are many people not taking GLP-1s who could still benefit from a wellness initiative.
A strong strategy is designed with this in mind. It meets people where they are and offers flexible options that can shape to any population’s needs. That kind of adaptability is essential to long-term effectiveness.
If you’re building for the long-haul, start here
For any weight-management strategy, the goal isn’t just to keep up. It’s to stay ahead. The strongest programs aren’t just reacting on defense as engagement drops, outcomes fall short, or costs creep up. They’re built to play offense— ready to adapt to evolving benefits and population needs.
Here are the questions worth asking:
- Does it support people throughout the full GLP-1 journey—including those who stop or never start?
- Can it help prevent the conditions that drive cost and complexity, like type 2 diabetes and high blood pressure?
- Are there tools built in to support behavior change and nutrition—not just at onboarding, but long term?
- What happens after the first 90 days, when initial motivation starts to dip?
- Are you measuring more than weight—like medical claims, sustained engagement, and daily quality of life?
- Is this something your team will feel good about a year from now—not just something that checks a box today?
A good strategy should feel solid when you launch it. A great one still holds up when things get messy.
Final thought: Medication can accelerate, but behavior change sustains.
GLP-1s have opened new possibilities in obesity and chronic condition care. But they don’t teach people how to respond to setbacks or maintain progress when life gets complicated. That’s where behavior change comes in.
It’s the foundation that helps people build habits, navigate transitions, and stay engaged—on medication or not. And it’s the layer that makes your investment in access actually pay off.
At Wondr Health, we partner with employers and health plans to deliver sustainable, behavior-based solutions that flex with evolving medication use and real-world needs. Our programs are designed to last—and built to show measurable impact.
If you’re building for more than just the next benefits cycle, we’d love to help.