With the cost of chronic conditions making up 90% of total U.S. health-care spending, it’s no surprise that they are a top driver of employer health-care expenses. The good news? With the right chronic condition management tools, employers can improve employee well-being and their bottom line. By focusing on behavior-driven solutions, organizations can lower insurance premiums, enhance productivity, and foster a healthier workforce.
And employees agree. According to our latest survey, effective chronic disease management doesn’t just happen in a doctor’s office—it starts with daily behaviors.
Survey findings: What employees want for chronic condition management
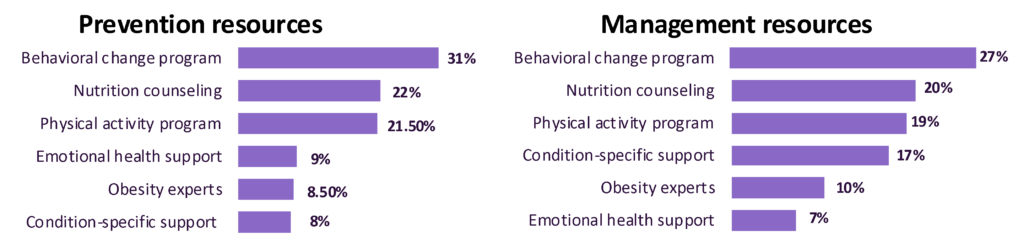
Prevention: Employees ranked behavioral change programs as the most effective way to prevent chronic conditions (31%), ahead of nutrition counseling (22%) and physical activity programs (21.5%).
Management: When managing conditions like diabetes, heart disease, or chronic pain, employees again ranked behavioral change as the #1 tool (27%), reinforcing its role in improving long-term health.
4 takeaways for a smarter chronic condition management strategy
By incorporating a proven behavior-change program within their wellness benefits, employers can improve the health of their people and their organization:
- Prevention is much more cost-effective than disease management. Better health isn’t just good for employees—it’s a smart business strategy. Investing in chronic disease prevention programs reduces high-cost claims before they happen.
- Behavioral change enhances treatment success. While there are additional tools that can improve employee health and well-being (such as GLP-1s), there can be a lack of support for employees taking these medications. Whether employees self-pay or use employer-covered weight-loss medications, combining treatment with lifestyle interventions leads to better adherence and outcomes.
- The ROI of chronic condition management is clear. The data is clear. Comprehensive workplace wellness programs rooted in behavior change have a direct impact on health-care expenses and they can also indirectly improve productivity, engagement, and workplace culture.
- Targeted chronic condition support improves outcomes. A solution that includes disease-specific resources—such as tailored interventions for diabetes, heart disease, and musculoskeletal conditions—ensures employees get the right support to manage their condition effectively, leading to better health outcomes and cost savings.
The bottom line of chronic condition management
With healthcare costs on the rise, employers can address the cost of chronic conditions with the right strategy. By providing comprehensive chronic disease support rooted in behavior change, businesses can improve employee well-being, build a healthier workforce, and strengthen their bottom line.
Want to know how we can help address the root cause of chronic disease? Let’s talk. You can reach us at https://wondrhealth.com/get-started-business/.